What does it mean when your optometrist says:
• your eyes are healthy, and you have 20/20 vision?
• here is your prescription for your glasses?
While different optometrists have different sets of expertise, and each one has different types of practices, the bread-and-butter of it is focused on assessing Visual Integrity.
In Contrast, Behavioural Optometry…
- Deals with improving the integrity, efficiency and processing of your vision.
- Studies estimate more than 50% of the brain’s function is involved with vision.
- This means that any neurological injury, such as a concussion, can result in a visual dysfunction.
What if your optometrist gets you to 20/20?
Or, you are already at 20/20?
But you still have symptoms like:
-
- Headaches
- Dizziness
- Nausea
- Light sensitivity
- Blurred vision
- Double vision
- Eye strain, fatigue, or “pulling/tugging” sensation around the eyes
- Difficulty with reading/computer work
- Difficulty with reading comprehension
- Inability to sustain near work or reading for periods of time
- Difficulty copying or taking notes
- Slow shift of focus from near-to-far or far-to-near
- Difficulty with concentration and attention
- Inability to tolerate busy or crowded environments
- Confusion or disorientation
- Difficulties with balance or coordination
- Clumsy or bumping into objects when walking
- A sensation of the floor, ceiling, or walls tilting
- A sensation of not feeling grounded
- Postural shifts/veering off when walking
- Difficulty with memory
What could be going on?
The visual system can be conceptually seen as being comprised of 4 rungs in a pyramid:
- Basic Visual Exam/Visual Integrity
- Non-vision based problems
- Non-oculomotor based problems/Visual Processing
- Oculomotor-based problems/Visual Efficiency
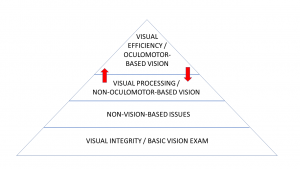
Connection Between the 4 Levels
Our experience has shown us that the hierarchy in rehabilitation visual issues post-concussion is as depicted above:
rungs lower down in the pyramid need to be addressed first in order to efficiently tackle upper levels.
The red arrows signify that there is a strong interdependent relationship between the 3rd and 4th tiers of this pyramid.
In fact, although the bottom level is the foundation for what lays above, all levels are interdependent on one another.
A practical example would be that, progressive lenses are commonly given to patients in the non-concussion population, but progressive lenses are usually not recommended in concussion patients (Jean-Louis et al., 2015).
We present the these four rungs of the pyramid in a different order as we find it is more intuitive for patients to understand it in the way we present it.
• This is the area where most optometrists spend most of their time.
Ocular Health
• They ensure that your eyes are structurally healthy and that there are no signs of disease.
Refraction
• If you need it, they ensure that they can give you lenses to bring you to 20/20, both when looking near, far, and in-between
-
- Common issues here in mTBI are increased myopia (near-sightedness) or new/increased hyperopia (far-sightedness) (Jean-Louis et al., 2016).
- This may be due to an abnormally functioning autonomic nervous system, a common consequence of concussion.
- There are many ways to train the autonomic nervous system including exercise and biofeedback-based interventions.
- Glasses may be required for refractive issues deemed to be “minor” in the non-concussion population (see article on Glasses & Rehabilitation)
- This is because methods we use to compensate for slight blurriness may not be “on-line” in post-concussion syndrome.
- Patients with Visual Processing issues like vestibular dysfunction or visual motion sensitivity usually don’t tolerate progressive addition lenses (Jean-Louis et al., 2015).
- Common issues here in mTBI are increased myopia (near-sightedness) or new/increased hyperopia (far-sightedness) (Jean-Louis et al., 2016).
• They may help with symptoms you may be having like dry eye, etc.
Binocularity
• Some patients have difficulty seeing out of both eyes at the same time, and many don’t realize it as such, they just recognize symptoms.
-
- Optometrists will often prescribe more specialized lenses or modification to your lenses to help you get on with things until you are able to rehabilitate the issue and no longer need the glasses.
Why the Need to Check More Than This?
• However, most optometrists do not check the next three rungs higher up on this pyramid.
• A simple way to think about it so to reflect on how they examine your eyes.
-
- Usually you are seated without moving your head
- You are a fixed distance from a chart that is not moving
- There are no distracting things going on
- Lighting is ideal
- You have a lot of time to focus on what you’re looking at
- The things you are looking at have been calculated to be precise and accurate
One will notice that this doesn’t match the way we use our eyes in every day life.
• For the most part, if we can get you to 20/20 vision, then we assume visual efficiency and processing is fine.
• This assumption is true for most of the population which is why we get away with it.
• This assumption, however, is not true for post-concussion patients.
• Hence, we have to check the next three levels – Oculomotor based-vision/Visual Efficiency & Non-oculomotor-based vision/Visual Integrity – when investigating post-concussion patients’ symptoms.
• Often, a specialized optometrist, specializing in this area handles this.
Many who have sustained a concussion continue to have 20/20 vision yet still experience visual symptoms due to a disruption in their binocular vision.
It has been reported that 90% of patients in a concussion clinic reporting “visual symptoms” had one or more oculomotor deficits (Ciuffreda et al., 2007).
- Binocular vision is the ability to use both (bi) eyes (ocular) together effectively at the same time.
- The efficiency of the visual system influences how we collect and process information.
- In order to do this, we need our “visual skills” to work at their optimal levels.
These visual skills include:
1. Saccades
-
- being able to jump your gaze accurately from one thing to another.
2. Fixation
-
- keeping objects in focus.
3. Pursuits:
-
- involves tracking an object by smoothly moving your eyes while keeping the target in focus.
4. Vergence
-
- as things get further from your eyes, your brain tells your eyes to pull apart, or diverge
- when you look at something closer up, your brain tells your eyes to cross the eyes, or converge
- Read our articles on Convergence Excess and Convergence Insufficiency to learn more about this system.
5. Reading
-
- We put this here since it’s such an important everyday thing we do.
- Generally, reading rate reduces by about 25% (Ciuffreda et al., 2007).
- And the number of times patients have to jump their gaze over to the next word and bring it into focus increased by about 20% (Ciuffreda et al., 2007).
6. Accommodation
-
- You can learn more about accommodation by reading the article Accommodative Dysfunction.
The efficiency of these visual systems and how well they work with each other influences how we collect and process visual information.
Once a visual image is captured by the eyes and teed up to the brain, what kinds of things are involved?
What could go wrong?
1. Abnormal Egocentric Localization
-
- Your perception of straight ahead looks off, like it has been rotated.
- This can cause you problems with feeling out of sync when you’re walking, or thinking objects are somewhere and they are actually a bit off from where you marked them.
2. Photosensitivity
-
- To oversimplify it, this refers to an aversion to light.
- Read more in our article on Light Sensitivity.
3. Visual Motion Sensitivity (VMS)
-
- This is when things you see reduces your sense of stability.
- Visual stimuli that trip up patients with VMS include wide (occupying most of your field of view) repetitive patterns (like tiles in a museum); busy, haphazard scenes (e.g., flea market, supermarkets); visual scenes whizzing by (e.g., think being a passenger in a car), etc.
- Progressive addition lenses is usually not recommended (Jean-Louis et al., 2015)
- Read more in our article Visual Vestibular Mismatch.
4. Vestibular Dysfunction.
-
- Read our articles:
- Progressive addition lenses is usually not recommended (Jean-Louis et al., 2015)
- Listen to our podcast:
5. Visual Field Defects
-
- When you can’t “see” portions of your field of view.
6. Visual Information Processing Dysfunctions
-
- things like processing delays and processing errors of visual information
- To be able to visually scan a crowd and pick out the thing of interest (E.g., think “Where’s Waldo” books)
Many of our patients come wanting to get right into vision therapy, but more gains are to be had by starting in rehabilitating these conditions first. See more in our video “Why not Start with Vision Therapy?”
This involves evidence-based methods of retraining visual efficiency and visual processing ability.
It also involves “crutches”; things like (Ciuffreda et al., 2002):
-
- corrective lenses
- prisms
- tints and coatings
- selective occlusion
Optimal rehabilitation of the neuro-visual system involves treating/optimizing many other health issues too, as we will discuss in the next section.
There are many non-vision-based problems that are very important to treat if NVR is to be successful.
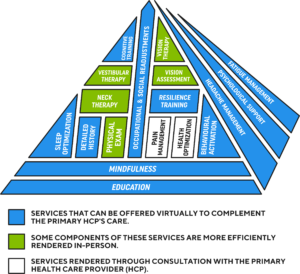
The following diagram illustrating the general way our program is organized
-
- It shows the interdependent and hierarchal relationship between the visual system and other parts of the concussion-recovery puzzle.
Some common areas that have been shown to affect visual system recovery in post-concussion patients include:
1. Depression
-
- People who are depressed are less likely to be motivated to do the therapy, let alone do it effectively.
- There are cognitive and autonomic dysfunction implications with depression which can get in the way of therapy.
- Energy level tends to be low.
- Read more in our article on Depression.
- Check out our podcast episodes “The Glass is Half Full” and “Down but not out“
2. Fatigue
-
- Check out our podcast episodes “To Rest or not to Rest“
- Read more about Fatigue
3. Cognitive Impairment
-
- Read our articles on cognition:
4. Postural Problems
-
- In our experience, this is a very important foundational step to effectively treating post-concussion visual issues.
- Check out our video on this: “Why not Start with Vision Therapy?”
- Read more in our article Visual Vestibular Mismatch
5. Neurological
-
- The most common issue that complicates post-concussion vision rehabilitation are post-traumatic headaches (PTH)
- PTH are treated with several different treatments.
- treatments of PTH are broad and span behavioural, lifestyle and medical approaches.
- check out our library for several articles on headaches.
- Poorly managed headaches makes vision therapy difficult as vision therapy often triggers headaches in these patients that make it difficult for them to participate in rehabilitation.
- Not too often, but occasionally, other neurological issues get in the way of recovery. Conditions like functional movement disorders.
Ciuffreda KJ. The scientific basis for and efficacy of optometric vision therapy in non- stra- bismic accommodative and vergence disorders. Optometry 2002;73:735–62.
Ciuffreda KJ, Kapoor N, Rutner D, et al. Occurrence of oculomotor dysfunctions in acquired brain injury: a retrospective analysis. Optometry 2007;78:155–61.
Jean-Louis É. Traumatic brain injury. Aide Soignante. 2016;30(173):31-32. doi:10.1016/j.aidsoi.2015.11.009
Last update: February 2021
